As we reach the age of wisdom, a peculiar dental phenomenon often arises—the eruption of our third molars, or the wisdom teeth. These teeth are the last set of teeth to emerge, and are often a source of dental issue due to impaction. While some can live in harmony with their wisdom teeth, many suffer from discomfort caused by the emergence of the teeth. Among these issues, an unsettling occurrence may manifest: jaw popping. But is the wisdom teeth the reason behind jaw popping, or TMJ?
The answer is NO, the existence or removal of the wisdom teeth does not cause TMJ disorder to occur as the teeth are no where near where the jaw popping is found. Extracting a wisdom teeth will not eliminate the symptoms of a TMJ disorder. If any, it is a mere coincidence.
In this article, we will take a deep dive into what TMJ disorders are, and why it is often associated with the eruption or removal of the wisdom teeth. By delving into the complexities of impacted wisdom teeth and their interaction with the jaw, we hope to shed light on why some people experience jaw popping while others remain unaffected.
Understanding TMJ disorders
TMJ disorders, also known as temporomandibular joint disorders (TMD), are a group of conditions that affect the jaw joint and surrounding muscles, causing discomfort and impairment in daily activities like chewing and speaking. These include:
- TMJ muscles – lateral pterygoid, medial pterygoid, temporalis, masseter
- Mandibular fossa of the temporal bone
- Condylar (Condyle) head of mandible
- Articular disc
The temporomandibular joint is akin to a hinge, connecting your jawbone to your skull and facilitating essential movements like chewing, speaking, and yawning. TMD, which affects millions of people annually, occurs when the joint is impaired.
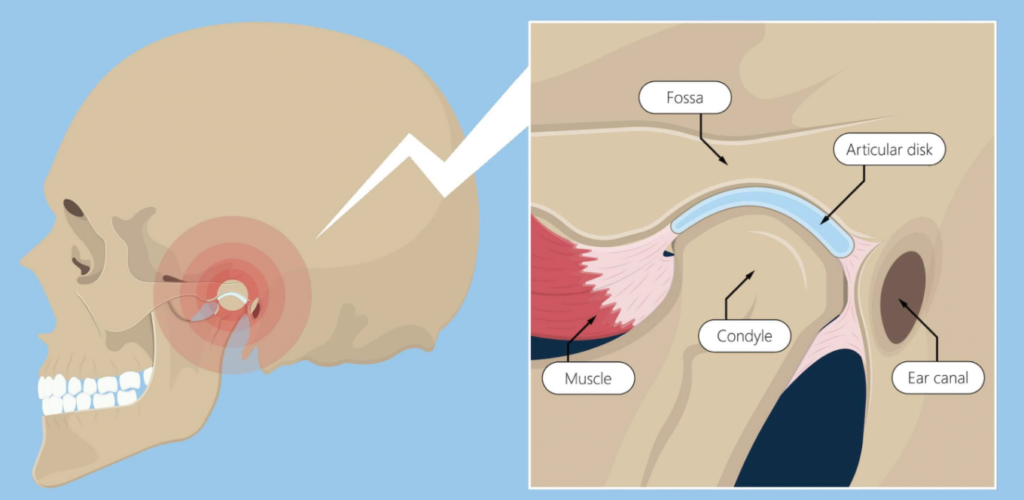
Symptoms of TMJ disorders may manifest as jaw pain, tenderness, clicking or popping sounds when opening or closing the mouth, difficulty chewing, headaches, and earaches.
Understanding the causes of TMJ disorders is crucial in identifying potential triggers and seeking appropriate treatment. Some of the factors that can cause TMD include:
- Malocclusion: Misalignment of the teeth and bite problems can place undue stress on the jaw joint during chewing and other movements, leading to TMJ-related symptoms.
- Bruxism (Teeth Grinding): Habitual teeth grinding or clenching, especially during sleep or times of stress, can strain the jaw joint and surrounding muscles, contributing to TMJ disorders.
- Trauma or Injury: Physical trauma to the jaw, such as accidents or impact injuries, can damage the TMJ and cause chronic discomfort.
- Arthritis: Inflammatory joint conditions, such as rheumatoid arthritis or osteoarthritis, can affect the temporomandibular joint and lead to pain and restricted movement.
- Stress: Chronic stress can cause increased muscle tension in the jaw and face, exacerbating TMJ-related symptoms.
- Genetics: Some individuals may be predisposed to TMJ disorders due to genetic factors that affect jaw structure and function.
- Poor Posture: Maintaining improper posture, especially in the neck and upper back, can affect the alignment of the jaw and contribute to TMJ problems.
While the wisdom teeth is a source of discomfort for many, it does not contribute to TMJ disorder. However, it is often misidentified as the cause of TMD due to the dental problem it is causing.
You may be interested in: Is It Possible to Have 8 Wisdom Teeth and Why?
Jaw Popping After Wisdom Teeth Removal
Many individuals who had their wisdom teeth removal surgery reported experiencing jaw popping, leading them to suggest that TMJ disorder is caused by the extraction of the teeth. This is sometimes the case, where TMJ disorder is a complication from the surgery. In a 2014 study conducted by the School of Dentistry, University of Washington, it was revealed that as much as 30% of the patients reported joint pain after the wisdom teeth removal surgery.
That said, more often than not, patients associate the general pain after the surgery with TMJ disorder. This is known as “referred pain”, and may have been the reason for the high percentage of reported TMJ disorder after a wisdom teeth removal surgery.
If you are experiencing jaw popping after wisdom teeth removal, note that it is temporary and should subside as the recovery progresses. During the first week after your surgery, adhere to the following instructions:
- Apply ice packs: Apply cold ice packs on the swollen area to reduce swelling and ease the muscle tension
- Go on a soft diet: As far as possible, stick to a soft diet to minimize jaw movement and reduce the risk of a dry socket. Some of the recommended food include soups, scrambled egg, mash potatoes, and yogurt. See here for a full list of soft food you should have and avoid.
- Have gentle jaw exercises: Performing gentle jaw exercises recommended by your dentist or oral surgeon can help improve jaw mobility and alleviate symptoms.
- Avoid chewing on the extraction side: Refrain from chewing on the side where the wisdom teeth were removed to avoid additional strain on the jaw.
- Have pain medications: If you are prescribed pain relief medications feel free to have them as instructed by your dentist. You may be given antibiotics if your dentist have deemed it necessary.
If the symptoms persist or worsen over time, it is essential to consult with the oral surgeon or dentist who performed the extraction.
Treatment Methods for TMJ Disorders
The management of TMJ disorders often involves a combination of conservative approaches and, in more severe cases, more invasive interventions. Also, depending on the potential cause of TMJ disorder, you may need to adopt different interventions.
Self-Care and Lifestyle Modifications: One of the most common steps in TMJ disorder management involves self-care and adjustments to your current lifestyle. Resting the jaw by avoiding hard or chewy foods and minimizing excessive jaw movements can help reduce strain on the temporomandibular joint (TMJ). Applying ice packs and warm compresses to the affected area can also help reduce inflammation and ease muscle tension. Additionally, stress management techniques such as relaxation exercises, mindfulness practices, and stress-reducing activities can be beneficial in relieving jaw clenching or teeth grinding caused by stress.
Medications: Pain relievers, such as over-the-counter medications like ibuprofen or acetaminophen, can help manage mild to moderate TMJ pain. Muscle relaxants may be prescribed to alleviate muscle spasms and reduce jaw tension, especially in cases where muscle-related symptoms are prominent.
You may be interested in: Can I Drink Coffee After Wisdom Teeth Removal?
Oral Splints or Mouthguards: Custom-fitted oral splints or mouthguards are often recommended by dentists to address jaw misalignment, prevent teeth grinding, and reduce stress on the TMJ. These devices help to stabilize the jaw and create a proper bite alignment, relieving pressure on the joint and surrounding muscles.
Physical Therapy: Physical therapy plays a significant role in TMJ disorder treatment. Physical therapists can design specific exercises to strengthen and stretch the jaw muscles, improving jaw mobility and reducing discomfort. These exercises, when done correctly and regularly, can enhance the range of motion and functionality of the TMJ.
Transcutaneous Electrical Nerve Stimulation (TENS): TENS therapy involves the use of low-level electrical currents to stimulate the TMJ area. The therapy provides pain relief and helps relax the jaw muscles, contributing to reduced discomfort and improved jaw function.
Dental Treatments: Dental professionals may offer various treatments to address TMJ disorders. Bite adjustment, involving selective grinding or reshaping of the teeth, can correct bite issues and reduce TMJ strain. Additionally, dental restoration, such as crowns or bridges, can improve bite alignment and alleviate TMJ discomfort caused by dental issues.
Counseling and Behavioral Therapies: Cognitive Behavioral Therapy (CBT) can be beneficial for managing stress and anxiety related to TMJ disorders. This form of therapy helps individuals develop coping strategies and behavioral modifications to reduce habits like jaw clenching or teeth grinding.
Surgery: In severe and refractory cases of TMJ disorders, surgical interventions may be considered. Arthrocentesis, a minimally invasive procedure involving the insertion of needles into the joint to irrigate and remove debris, can provide relief. Arthroscopy, a surgical procedure using a small camera to diagnose and treat TMJ disorders, may be used for more complex cases. Open joint surgery, which involves open access to the TMJ to repair or replace the joint, is reserved for severe and rare instances.
Before engaging in any of the above interventions, always consult with a qualified dental or healthcare professional for an accurate diagnosis and personalized treatment plan. Remember, early intervention and the right treatment recommendations can significantly improve your TMJ health and overall well-being.
Concluding Thoughts
The question of whether wisdom teeth can cause jaw popping or TMJ is one that has intrigued many individuals dealing with dental issues. As explained, the positioning of the wisdom teeth does not lead to TMJ disorder because it is not associated with the TMJ.
Prompt intervention is crucial in addressing wisdom teeth-related jaw popping or TMJ problems. Seeking professional dental care and evaluation by a dentist or oral surgeon is essential in diagnosing the issue accurately. Based on the evaluation, appropriate treatment options can be recommended, including wisdom tooth extraction if they are causing significant problems.